Alzheimer's disease
Definition
Alzheimer's disease, or AD, is a progressive, incurable disease of the brain caused by the degeneration and eventual death of neurons (nerve cells) in several areas of the brain.
Description
Patients with AD first lose such mental functions as short-term memory and the ability to learn new things. In the later stages of AD they gradually lose control over their sense of orientation, their emotions, and other aspects of behavior. End-stage AD is characterized by loss of control of body functions, an increased likelihood of seizures , loss of the ability to eat or swallow, and eventual death from infection or malnutrition. Alzheimer's disease is the most common cause of dementia (loss of cognitive abilities) in the elderly; it is thought to be responsible for 50%–70% of cases of dementia in the United States.
Alzheimer's disease was first identified in 1906 by a German psychiatrist and neuroanatomist named Alois Alzheimer. He was studying slides prepared from the brain of a fifty-one-year-old woman, known as Frau D., who had died after several years of dementia with symptoms that did not fit the definition of any brain disorder known at the time. Alzheimer was the first to describe the plaques and neurofibrillary tangles that are now used to identify AD at autopsy. Plaques are clumps or clusters of dead or dying nerve cells and other cellular debris found in the brains of patients with Alzheimer's disease. Neurofibrillary tangles are the accumulations of twisted protein fragments found inside the nerve cells in the brains of Alzheimer's patients. Because dementia had been associated with elderly people and Frau D. had been middle-aged, AD was first known as presenile dementia and was thought to be a very rare disorder. It was not until the early 1950s that researchers at St. Elizabeth's Hospital in Washington, DC, came to recognize that AD is the single most common cause of dementia in adults.
Alzheimer's disease is now considered a very serious public health problem because of the growing numbers of people who are affected by it, the increasing length of their lives, and the direct and indirect costs of their care. It is estimated that four million people in the United States had AD as of 2000, with 360,000–400,000 new cases identified every year. One person in ten over the age of 65 has AD, and nearly 50% of those over 85 have the disease. Unless a cure or preventive treatment is discovered, 14 million Americans will have Alzheimer's by 2050. Very few people are wealthy enough to cover the cost of caring for an Alzheimer's patient in the seven–10 years that typically extend between the beginning of the person's dependency and death. The average lifetime cost of caring for one patient with AD is estimated at $174,000. The costs of laboratory tests, physicians' visits, medications, nursing services, home care, and adult day care come to $114.4 billion per year in the United States alone. This sum is greater than the combined annual budgets of six Federal departments (Commerce, Education, Justice, Labor, Energy, and Interior).
The problem is expected to be complicated in future years by the fact that the so-called "baby boomer" generation is better nourished and better educated than the generation now at risk for AD. When the baby boomers are old enough to be at risk for late-onset Alzheimer's, they are expected to live longer than the average Alzheimer's patient does in 2002. Public health researchers who are making future projections about the impact of AD in the mid-twenty-first century point out that a treatment that would delay the onset of the disease would reduce the overall prevalence of AD. One study estimates that a therapy that would delay the onset of Alzheimer's by only one year would save the United States $9 billion by 2007. The second approach, that of discovering a treatment for people who already have Alzheimer's, would alter the proportion of mild cases to those considered moderate or severe. The researchers conclude by stating: "None of our models predicts less than a threefold rise in the total number of persons with Alzheimer's disease between 2000 and 2050."
Types of Alzheimer's disease
As of 2002, some researchers think that Alzheimer's may be more accurately described as a group or family of diseases rather than a single disease. Moreover, more recent research is helping to differentiate Alzheimer's disease from other less common causes of dementia. In particular, some cases of dementia that were formerly thought to have been related to AD are now known to have been caused by Pick's disease or Lewy body dementia. Pick's disease is a rare type of dementia that affects certain areas of the brain and is characterized by a progressive loss of social skills, language, and memory. Lewy body dementia is a type of dementia in which the brain has characteristic Lewy bodies—areas of injury found on damaged nerve cells in certain parts of the brain.
Physicians now recognize three different forms of Alzheimer's disease.
EARLY-ONSET AD. Early-onset AD is a rare form of Alzheimer's found in fewer than 10% of AD patients. This group of patients, however, develops more of the brain abnormalities associated with AD than patients with the late-onset form. In addition, patients with early-onset Alzheimer's are more likely to develop myoclonus (a condition in which a muscle or group of muscles has sudden spasms or twitching).
LATE-ONSET AD. Late-onset AD is the most common form of the disease; its symptoms usually begin to appear after age 65. Late-onset Alzheimer's, which may or may not be affected by genetic variables, is also called sporadic Alzheimer's disease because it does not necessarily run in families.
FAMILIAL ALZHEIMER'S DISEASE (FAD). Familial Alzheimer's disease, or FAD, is a rare form that is entirely inherited. FAD accounts for fewer than 5% of all cases of AD. It has a very early onset, often in the patient's 40s, and there is a clear family history of the disease.
Stages
Health care professionals use the term "insidious" to describe Alzheimer's, which means that it is very gradual in onset. Many times people recognize the first symptoms of the disorder in a friend or family member only in hindsight. In addition, the present generation of people old enough to be at risk for Alzheimer's is the first generation in history to know what the diagnosis means; there are therefore very powerful emotional reasons for attributing the early signs of AD to normal aging, job stress , adjusting to retirement, and other less troubling factors. The insidious onset of Alzheimer's is a characteristic, however, that allows doctors to distinguish it from other causes of dementia, including vascular dementia .
EARLY-STAGE ALZHEIMER'S. Early-stage Alzheimer's may begin almost imperceptibly. The first symptoms usually include short-term memory loss, temporary episodes of spatial disorientation, groping for words while one is speaking, minor problems with arithmetic, and small errors of judgment. For example, the person may light a stove burner under a saucepan before noticing that he has forgotten to put the food or water in the pan first, or he may have difficulty balancing a checkbook as quickly as he used to. At this stage in the disease, however, the patient can usually keep up with most activities of daily life. Although some persons at this point can still operate a motor vehicle safely, it is advisable to consult a physician about possible impairment behind the wheel. Many patients with early-stage AD voluntarily give up their driver's licenses for their own safety and that of other drivers on the roads.
MIDDLE-STAGE ALZHEIMER'S. In the middle stage, which typically begins two to three years after onset, the person begins to lose awareness of his or her cognitive deficits. Memory lapses are more frequent and the person begins to have more severe problems with language. Unlike early-stage AD, the problems caused by loss of cognitive functioning are impossible to ignore. The middle stage of AD is the point at which the behavioral and psychiatric symptoms that are so stressful to caregivers often begin— the agitation, wandering, temper outbursts, depression, and disorientation. The patient is at high risk for falls and similar accidents. In addition, the patient becomes increasingly unable to understand simple instructions or to follow a conversation, and begins to lose his or her basic sense of personal identity.
END-STAGE ALZHEIMER'S. End-stage Alzheimer's is marked by the loss of the ability to walk and eventually even to sit up. Patients may be able to use a wheelchair for awhile but eventually become completely bedridden. They lose bladder and bowel control. When the disease begins to affect the patient's brain stem, the basic processes of digestion, respiration, and excretion shut down. Patients usually stop eating at this point and sleep most of the time. The hands and feet begin to feel cold, the breathing becomes shallow, and the patient is generally unresponsive to caregivers. Eventually the patient's breathing simply stops.
Causes and symptoms
Causes
Evidence has accumulated that Alzheimer's disease is multifactorial— that is, it is caused by a combination of several genetic and environmental factors.
GENETIC. Early-onset AD is caused by a defect in one of three genes known as APP, presenilin-1, and presenilin-2, found on human chromosomes 21, 14, and 1, respectively. Early-onset AD is also associated with Down syndrome, in that people with trisomy 21 (three forms of human chromosome 21 instead of a pair) often develop this form of Alzheimer's. The brains of people with Down syndrome age prematurely, so that those who develop early-onset AD are often only in their late 40s or early 50s when the symptoms of the disease first appear.
Genetic research indicates that late-onset Alzheimer's disease is a polygenic disorder; that is, its development is influenced by more than one gene. It has been known since 1993 that a specific form of a gene for apolipoprotein E (apoE4) on human chromosome 19 is a genetic risk factor for late-onset AD. People who have the apoE4 gene from one parent have a 50% chance of developing AD; a 90% chance if they inherited the gene from both parents. They are also likely to develop AD earlier in life. One of the remaining puzzles about this particular gene, however, is that it is not a consistent marker for AD. In other words, some people who have the apoE4 gene do not develop Alzheimer's, and some who do not have the gene do develop the disorder. In 1998 another gene on chromosome 12 that controls the production of bleomycin hydrolase (BH, an enzyme involved in the body's processing of amyloid precursor protein) was identified as a second genetic risk factor that acts independently of the APOE gene. In December 2000, three separate research studies reported that a gene on chromosome 10 that may affect the processing of a particular protein is also involved in the development of late-onset AD.
Familial Alzheimer's disease appears to be related to abnormal genes on human chromosomes 21 and 14.
NEUROBIOLOGICAL. Investigators since Alois Alzheimer's time have studied the abnormalities found at autopsy in the brains of patients with AD. One abnormality is plaques, or clumps, of a starchy protein called beta amyloid. Beta amyloid is formed when a substance called amyloid precursor protein, or APP, fails to be metabolized properly in the body. APP is a substance found in many parts of the body, but its precise function is not yet known. Following the formation of beta amyloid, pieces of it then stick to one another and gradually build up into plaques. The other abnormal finding is neurofibrillary tangles, which are twisted threads formed from parts of the dying nerve cell called the tau protein, which was discovered in 1986. If the tau protein is damaged by the addition of molecules of phosphorus, a process called hyperphosphorylation, it forms filaments that twist around each other to form the neurofibrillary tangles. As the plaques and tangles accumulate in the brain, they cause the nerve cells to wither and eventually die. As the nerve cells die, the affected parts of the brain start to shrink in size. It is not known as of 2002, however, whether the plaques and tangles are causes of AD or results of it. The relationship between the plaques and the tangles is another question that has not yet been answered. Although the plaques usually appear in brain tissue before the tangles, it is not clear that they cause the tangles. There are other brain disorders, such as Pick's disease, in which tangles appear in the brain cells without plaques.
Another nervous system abnormality in AD is the lowered level of neurotransmitters produced by the cells in the brain. Neurotransmitters are chemicals that carry nerve impulses across the small gaps (synapses) between nerve cells. The neurotransmitters whose production is affected by Alzheimer's include serotonin, norepinephrine, and acetylcholine. Many of the behavioral and psychiatric problems associated with AD are thought to result from the inadequate supply of these neurotransmitters.
ENVIRONMENTAL. Researchers have been studying the possibility that certain chemicals or other toxins in the environment may have a role in causing or triggering AD. The environmental factors that have been considered include aluminum, zinc, toxins in contaminated food, and viruses. Although there is little evidence as of 2002 that AD is caused by a virus or other infectious agent, the possibility cannot be completely excluded.
Other hypotheses about the causes of Alzheimer's include damage caused by oxidation, estrogen deficiency, and inflammation. All of these possibilities are presently under investigation.
RISK FACTORS. A number of factors have been identified that increase a person's risk of developing Alzheimer's:
- Age. The risk of developing AD rises after age 65, and rises sharply after age 75. While 1% of the population has AD at age 65, almost 50% of those over 85 have it.
- Sex. Women are more likely to develop AD than men. As of 2002, however, it is not known whether women are more susceptible to the disorder, or more likely to develop it because they live longer than men, on average.
- Family history of AD.
- Having Down syndrome.
- History of head injury.
- Substances in the environment. Higher-than-average amounts of aluminum have been found in the brains of patients with Alzheimer's. Some researchers in the late 1990s thought that exposure to aluminum might be a risk factor for the disorder. It now appears that the levels of aluminum in the brains of patients are a result rather than a cause of AD.
- Low occupational attainment and education level. Studies have found a clear correlation between employment in jobs that are not mentally challenging and an increased risk of AD. In addition, taking less rather than more challenging jobs as one grows older is associated with a higher risk of AD.
- High systolic blood pressure.
- High blood cholesterol levels. When both high systolic blood pressure and high cholesterol are present, the risk of developing AD increases by a factor of 3.5.
- Mild cognitive impairment (MCI). Mild cognitive impairment is a transitional decline in cognitive functioning that precedes the onset of AD. MCI is characterized primarily by memory loss while other cognitive functions remain intact. People with MCI are at higher risk for AD than people who do not develop the condition; 12% of people with mild cognitive impairment develop Alzheimer's disease each year, compared with 1–2% per year of people without MCI. After four years, 40% of people diagnosed with mild cognitive impairment have clear symptoms of Alzheimer's disease.
Symptoms
The symptoms of Alzheimer's can be grouped into three categories: cognitive deficits, or losses of brain function related to memory and learning; behavioral and psychiatric symptoms of dementia, or BPSD; and problems with activities of daily life, or ADLs.
COGNITIVE DEFICITS. There are four major symptoms of loss of cognitive capacities in Alzheimer's:
- Amnesia . Amnesia refers to memory impairment; however, loss of short-term memory also means that the patient loses his or her sense of time as well.
- Aphasia. Aphasia refers to loss of language function. The person may not remember the names of objects and may use words like "thing" or "it" instead; they may echo what other people say or repeat a word or phrase over and over. On occasion the person may lose the ability to speak except for curse words.
-
Apraxia. Apraxia is the loss of the ability to perform voluntary
movements in the absence of paralysis. A person with apraxia, for
example, may have trouble putting on a hospital gown or brushing his or
her teeth.
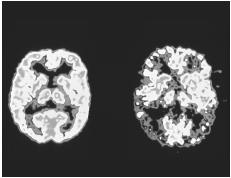
 A brain segment affected by Alzheimer's disease on the right compared with a healthy brain segment (left). The brain affected by disease appears shrunken, and the fissures are noticeably larger.(Simon Fraser/MRC Unit, Newcastle General Hospital/Science Photo Library. Photo Researchers, Inc. Reproduced by permission.)
A brain segment affected by Alzheimer's disease on the right compared with a healthy brain segment (left). The brain affected by disease appears shrunken, and the fissures are noticeably larger.(Simon Fraser/MRC Unit, Newcastle General Hospital/Science Photo Library. Photo Researchers, Inc. Reproduced by permission.) - Agnosia. Agnosia comes from a Latin word that means "to not know", and refers to inability to recognize familiar places and people. Patients with agnosia may even fail to recognize their own face in a mirror.
NEUROPSYCHIATRIC SYMPTOMS. Symptoms associated with BPSD include:
- Depression. Depression associated with AD is thought to result from the lowered production of the neurotransmitter serotonin. Depression in AD can be treated with medication, usually with one of the selective serotonin reuptake inhibitors, or SSRIs.
- Delusions . A delusion is a false belief that a person maintains even when presented with contrary evidence. For example, patients with AD may say that a person is stealing their things when they cannot remember where they have put them. Suspicions of other people caused by delusions can sometimes be treated with medication.
- Wandering. This behavior may result from becoming disoriented and getting lost, but sometimes people with AD wander for no apparent reason. The Alzheimer's Association in Chicago has a Safe Return Hotline (listed under "Resources," below) that can be contacted for information about registering a patient with AD. If the registered patient should wander from home, the Safe Return Hotline can help identify him or her and return them to their family or nursing home.
- Hallucinations . Like delusions, hallucinations in AD patients are thought to be related to the deterioration of the patient's brain tissue. In a hallucination, the patient has a sensory experience that is real to him or her but not to other people. Hallucinations can affect any of the senses, but most are either visual or auditory. For example, a patient with AD may say that he or she sees little Martians in the corner of the room, or that he or she hears the voice of a long-dead parent calling to them. Hallucinations are sometimes caused by medications that the patient may be taking.
- Aggression. Aggression refers to hitting, shoving, pushing, or threatening behavior.
- Agitation. Agitation refers to emotionally excited behavior (screaming, shouting, cursing, pacing, fidgeting, etc.) that is disruptive or unsafe. Agitation may result from the changes in the patient's brain tissue, or it may be a symptom of depression associated with Alzheimer's disease.
For most of the twentieth century, studies of Alzheimer's patients focused on the cognitive symptoms of the disorder. It was not until the 1980s and 1990s that researchers began to look more closely at the behavioral and psychiatric symptoms of AD. Such methods of standardized assessment of these symptoms as the neuropsychiatric inventory are very recent developments.
PROBLEMS WITH ACTIVITIES OF DAILY LIVING (ADLS). Needing help with ADLs, or personal care activities that are part of everyday living, is among the earliest symptoms of Alzheimer's. The functions that are often affected include:
- eating, including simple cooking and washing dishes
- bathing, showering, or shaving
- grooming and dressing in clothing appropriate to the weather and activity
- toileting
- other aspects of personal hygiene (brushing teeth or cleaning dentures, washing hair, etc.)
- shopping for groceries and other necessary items
Health care professionals usually assess the ADLs of a patient diagnosed with Alzheimer's in order to determine what type of care is needed.
Demographics
Some demographic statistics in the developed countries have already been cited in the context of risk factors for AD and public health concerns related to the disorder.
Relatively little is known about the demographics of AD and other forms of dementia in the developing countries. Alzheimer's Disease International, which is based in London, supports a group of researchers called the 10/66 Dementia Research Group. The 10/66 group is trying to correct the global imbalance of AD research; as of 2001, fewer than 10% of all population-based research studies of AD and related forms of dementia has been directed toward the 66% of people with these disorders who live outside the developed countries. Of the estimated 18 million people in the world with dementia, 12 million live in China, India, Latin America, and other developing nations.
Diagnosis
As of 2002, the diagnosis of AD is essentially a process of exclusion. The only definitive diagnosis of Alzheimer's is made post mortem (after death), by performing an autopsy and examining the patient's brain tissue. There are no present tests that can be done on a living person to make the diagnosis of AD more than probable.
Diagnostic evaluation of AD
At present, the diagnostic process includes the following components:
- Clinical interview. In the absence of laboratory tests or imaging studies that can provide definite diagnoses, the physician must rely on his or her clinical judgment. In evaluating the patient, the doctor will assess signs of cognitive impairment other than short-term memory loss. In most cases, the doctor will ask a family member or close friend of the patient about the suddenness of symptom onset and the length of time that the patient seems to have been impaired.
- Physical examination. The patient will be given a complete physical and have blood and urine samples taken to rule out vitamin deficiencies, head trauma, tertiary syphilis, thyroid disorders, and other possible causes of dementia. The doctor will also review all the medications that the patient is taking (including alternative remedies) in order to exclude reversible dementia caused by drug interactions.
- Neurological examination. In early AD, the neurological findings are usually normal. If the patient appears to have had a stroke , he or she will be referred for a more thorough assessment by a neurologist.
- Tests of cognitive function. The patient will be given the mini-mental status examination (MMSE) and such other tests of cognitive function as the clock test or verbal fluency tests. The MMSE is a screening test and should not be used by itself to make the diagnosis of AD. In addition, the MMSE is not very sensitive in detecting cognitive impairment in people who previously functioned at a high level and were well educated. It is possible for a well-educated person to score a perfect 30 on the MMSE and still suffer cognitive impairment. The clock test is a test in which patients are asked to draw a clock face. Sometimes, patients will also be asked to include a specific time on the clock, such as 3:20. Patients with Alzheimer's often draw the face of the clock with numbers out of order, or all of the hour markers in a portion of the clock face instead of evenly spaced around the face, and often have difficulty adding the clock hands.
- Neuropsychiatric evaluation. A neuropsychiatric examination may be given to determine the pattern of the patient's cognitive impairment and probe his or her level of functioning more deeply. The patient may be asked to write a sample check, to describe how they answer the phone, to interpret sample traffic signs, and to look at a shopping list and pick out the items on the list from a display.
- Diagnostic imaging. Imaging studies are useful in detecting such causes of dementia as a previously undiagnosed brain tumor or abnormal brain structure. Scans can show doctors that certain areas of the brain have lost tissue (as happens in AD), and can strengthen a physician's suspicion of a patient's AD diagnosis, but scans cannot diagnose AD on their own. Scans are used more to rule out other possible diagnoses and to confirm a suspected diagnosis. CT ( computed tomography ) scans are commonly performed, as well as MRI ( magnetic resonance imaging ) scans in patients who are having problems with gait or balance. PET ( positron emission tomography ) and SPECT ( single photon emission computed tomography ) scans can be used to evaluate patterns of glucose (sugar) metabolism in the brain and to differentiate the patterns that are characteristic of Alzheimer's from those associated with vascular dementia and Pick's disease. PET scans are more precise than SPECT scans, but their cost is prohibitive.
Ethical considerations
With regard to genetic factors, tests are now available for the apoE4 gene implicated in late-onset Alzheimer's, but the American College of Medical Genetics and the American Neurological Association do not recommend these tests as of 2002. One reason is that the test results are not conclusive— about 20% of people
Treatments
At present the mainstay of Alzheimer's treatment is medication, both to slow symptom progression and to manage the behavioral and psychiatric symptoms of AD.
Medications to slow symptom progression
The medications most commonly given to delay the progression of symptoms in Alzheimer's are a group of drugs called cholinesterase inhibitors. These drugs were approved by the FDA over a decade ago. They work by slowing down the body's destruction of the neurotransmitter acetylcholine.
The cholinesterase inhibitors include:
- Tacrine (Cognex). This drug is the oldest cholinesterase inhibitor in use. It is used less often than newer agents because it must be taken four times a day and may cause liver damage.
- Donepezil (Aricept). This drug is the one used most commonly as of 2002 to treat AD. It has fewer side effects than tacrine and can be given in one daily dose.
- Rivastigmine (Exelon). This drug is taken twice daily.
- Galantamine (Reminyl). This is the newest cholinesterase inhibitor, approved in late 2001. It acts on an additional acetylcholine receptor.
None of these medications provide more than modest benefits to patients with AD: they slow the progression of symptoms for about six months to a year in one-third to one-half of patients with AD. In addition, the cholinesterase inhibitors have side effects, most commonly nausea, vomiting, diarrhea, muscle cramps, and sleep disturbances.
Medications for BPSD
Medications are also prescribed to manage the behavioral and psychiatric symptoms of AD, which are often quite stressful for caregivers if the patient is being cared for at home. These medications are usually prescribed for specific symptoms:
- Delusions: Antipsychotic drugs, usually haloperidol (Haldol) or risperidone (Risperdal).
- Agitation: Short-term anti-anxiety drugs, usually lorazepam (Ativan) or buspirone (BuSpar).
- Depression: One of the selective serotonin reuptake inhibitors (SSRIs), at half the dosage for a young adult.
- Pain: Acetaminophen or a very low dose of codeine.
In general, older patients require lower dosages than those given to younger adults. Patients with AD are also more susceptible to the side effects of medications. For these reasons, physicians often recommend making changes in the patient's environment to reduce the behavioral symptoms before trying medications.
Alternative and complementary treatments
Some complementary therapies have been shown to benefit patients with Alzheimer's.
NATUROPATHY. A naturopathic approach to Alzheimer's includes supplementing antioxidant vitamins (vitamins A, E, and C) in the patient's diet, along with adding carotenoids, small amounts of selenium and zinc, and thiamin. Botanical supplements that have been said to improve cognitive function include Huperzine A, a Chinese tea, and an extract made from Gingko biloba , a tree that is native to China and is said to be the world's oldest living deciduous tree. GBE, or gingko biloba extract, is the most frequently used herbal medicine in Europe. It is available in Germany by prescription and in an over-the-counter form; and has been approved by the German Commission E for dementia-related memory loss. Gingko extract is thought to work in a manner similar to the cholinesterase inhibitors. At present the National Center for Complementary and Alternative Medicine (NCCAM) is conducting studies of gingko extract as a treatment for Alzheimer's.
MUSIC THERAPY. Music therapy has been found to calm agitated patients with Alzheimer's, to improve mood, and to enhance their long-term memory. Old familiar songs are particularly effective in improving recall. In other studies, music therapy has been shown to reduce sensations of chronic pain in patients with AD.
Prognosis
There is no cure for Alzheimer's disease as of 2002. The prognosis is progressive loss of mental and bodily functions leading to death within seven to ten years. Some patients, however, die within three years of diagnosis and others may survive for as long as fifteen.
Prevention
Researchers are considering several different strategies to prevent Alzheimer's, ranging from development of a vaccine to prevent the formation of beta amyloid plaques to finding a drug that would stop the conversion of APP to beta amyloid. As of 2002, the vaccine, which was originally developed and tested on mice, does not appear to have any serious side effects in humans. It is presently being tested in Phase II trials on human subjects.
See also Dementia ;
Resources
BOOKS
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th edition, text revised. Washington, DC: American Psychiatric Association, 2000.
Beers, Mark H., MD. "Behavior Disorders in Dementia." Chapter 41 in The Merck Manual of Geriatrics, edited by Mark H. Beers, MD, and Robert Berkow, MD. Whitehouse Station, NJ: Merck Research Laboratories, 2000.
Keck, David. Forgetting Whose We Are: Alzheimer's Disease and the Love of God. Nashville, TN: Abingdon Press, 1996.
Mace, Nancy L., and Peter V. Rabins. The 36-Hour Day. Revised and updated edition. New York: Warner Books, Inc., 2001; by arrangement with The Johns Hopkins University Press.
Marcantonio, Edward, MD. "Dementia." Chapter 40 in The Merck Manual of Geriatrics, edited by Mark H. Beers, MD, and Robert Berkow, MD. Whitehouse Station, NJ: Merck Research Laboratories, 2000.
Morris, Virginia. How to Care for Aging Parents. New York: Workman Publishing, 1996.
Pelletier, Kenneth R., MD. The Best Alternative Medicine. Part II. "CAM Therapies for Specific Conditions: Alzheimer's Disease." New York: Simon and Schuster, 2002.
Shenk, David. The Forgetting: Alzheimer's: Portrait of an Epidemic. New York: Doubleday, 2001.
PERIODICALS
Aisen, P. S., J. Schmeidler, G. M. Pasinetti. "Randomized Pilot Study of Nimesulide Treatment in Alzheimer's Disease." Neurology 58 (April 9, 2002): 1050-1054.
Bone, Kerry. "Gingko and Alzheimer's Disease." Townsend Letter for Doctors and Patients (January 2001): 27.
Desai, P. P., H. C. Hendrie, R. M. Evans, and others. "Genetic Variation in Apolipoprotein D Affects the Risk of Alzheimer's Disease in African Americans." American Journal of Human Genetics 69 (October 2001): 416.
Editorial Commentary. "Neuropsychiatric Phenomena in Alzheimer's Disease." Journal of Neurology, Neurosurgery and Psychiatry 71 (December 2001): 715.
"Head Injury Linked to Increased Risk of Alzheimer's Disease." FDA Consumer 35 (January-February 2001): 8.
Holmes, C., H. Smith, R. Ganderton, and others. "Psychosis and Aggression in Alzheimer's Disease: The Effect of Dopamine Receptor Gene Variation." Journal of Neurology, Neurosurgery and Psychiatry 71 (December 2001): 777-779.
in't Veld, Bas A., Annemieke Ruitenberg, Albert Hofman, and others. "Nonsteroidal Anti-inflammatory Drugs and the Risk of Alzheimer's Disease." New England Journal of Medicine 345 (November 22, 2001): 1515-1521.
Khosh, Farhang. "Naturopathic Approach to Alzheimer's Disease." Townsend Letter for Doctors and Patients (July 2001): 22-24.
Kim, S. Y., J. H. Karlawish, E. D. Caine. "Current State of Research on Decision-Making Competence of Cognitively Impaired Elderly Persons." American Journal of Geriartic Psychiatry 10 (March-April 2002): 151-165.
Kivipelto, M., and others. "Midlife Vascular Risk Factors and Alzheimer's Disease in Later Life: Longitudinal, Population-Based Study." British Medical Journal 322 (June 16, 2001): 1447-1451.
Langbart, C. "Diagnosing and Treating Alzheimer's Disease: A Practitioner's Overview." Journal of the American Academy of Nurse Practitioners 14 (March 2002): 103-109.
Luedecking-Zimmer, E., S. T. DeKosky, M. I. Kamboh. "Candidate Genes for Late-Onset Alzheimer's Disease on Chromosome 12." American Journal of Human Genetics 69 (October 2001): 518.
Moon, Mary Ann. "Mentally Demanding Work May Deter Alzheimer's Disease." Family Practice News 30 (September 1, 2000): 32.
O'Hara, R., and others. "Update on Alzheimer's Disease: Recent Findings and Treatments." Western Journal of Medicine 172 (February 2000); 115-120.
Olin, J. T., I. R. Katz, B. S. Meyers, and others. "Provisional Diagnostic Criteria for Depression of Alzheimer Disease: Rationale and Background." American Journal of Geriatric Psychiatry 10 (March-April 2002): 129-141.
Shah, Yogesh, Eric G. Tangelos, and Ronald C. Petersen. "Mild Cognitive Impairment: When Is It a Precursor to Alzheimer's Disease?" Geriatrics 55 (September 2000): 62-68.
Shigenobu, K., M. Ikeda, R. Fukuhara, and others. "Reducing the Burden of Caring for Alzheimer's Disease Through the Amelioration of 'Delusions of Theft' by Drug Therapy." International Journal of Geriatric Psychiatry 17 (March 2002): 211-217.
Silverman, Daniel H. S., Gary W. Small, Carol Y. Chang, and others. "Positron Emission Tomography in Evaluation of Dementia: Regional Brain Metabolism and Long-Term Outcome." Journal of the American Medical Association 286 (November 7, 2001): 2120.
Sloane, P. D., S. Zimmerman, C. Suchindran, and others. "The Public Health Impact of Alzheimer's Disease, 2000-2050: Potential Implication of Treatment Advances." Annual Review of Public Health 23 (2002): 213-231.
Walsh, D. M., I. Klyubin, J. V. Fadeeva, and others. "Naturally Secreted Oligomers of Amyloid Beta Protein Potently Inhibit Hippocampal Long-Term Potentiation in Vivo." Nature 416 (April 4, 2002): 535-539.
Wilcock, G. K., and others. "Efficacy and Safety of Galantamine in Patients with Mild to Moderate Alzheimer's Disease: Multicentre Randomised Controlled Trial." British Medical Journal 321 (December 9, 2000): 1445-1449.
ORGANIZATIONS
Alzheimer's Association. 919 North Michigan Avenue, Suite 1100, Chicago, IL 60611-1676. (800) 272-3900 or (312) 335-8700. Fax: (312) 335-1110. <www.alz.org> .
Alzheimer's Disease Education and Referral (ADEAR) Center. P. O. Box 8250, Silver Spring, MD 20907-8250. (800) 438-4380. <www.alzheimers.org> .
Alzheimer's Disease International. 45–46 Lower Marsh, London SE1 7RG, UK. (+44) 20-7620-3011. Fax: (+44) 20-7401-7351. <www.alz.co.uk> .
National Center for Complementary and Alternative Medicine (NCCAM) Clearinghouse. P.O. Box 7923, Gaithersburg, MD 20898. (888) 644-6226. TTY: (866) 464-3615. Fax: (866) 464-3616. <www.nccam.nih.gov> .
National Institute of Mental Health. 6001 Executive Boulevard, Room 8184, MSC 9663, Bethesda, MD 20892-9663. (301) 443-4513. <www.nimh.nih.gov> .
National Institute of Neurological Disorders and Stroke (NINDS). Building 31, Room 8A06, 9000 Rockville Pike, Bethesda, MD 20892. (301) 496-5751. <www.ninds.nih.gov> .
OTHER
Safe Return Hotline. (888) 572-8566. This hotline provides information about registering a patient with AD with the Alzheimer's Association as a means of identification in the event that he or she wanders away from home.
Rebecca J. Frey, Ph.D.
Comment about this article, ask questions, or add new information about this topic: