Psychosurgery
Definition
Psychosurgery is the treatment of a psychiatric disorder using surgical techniques to destroy brain tissue and is now rarely used.
Purpose
It is a last-resort treatment for extreme, debilitating, psychiatric disorders.
Description
Early psychosurgery—historical perspective
Ironically, brain surgery, a medical practice requiring extraordinary levels of skill and care, may be one of the oldest of all medical procedures. This surprising observation is supported by physical evidence dating back 40,000 years ago to Neolithic times. Archeologists have found numerous human skulls showing signs of a procedure called trepanation or trepanning—an operation in which a hole is cut through the bone that covers the brain (skull) in order to access the brain. A key feature of the wounds found in these ancient skulls is the smoothness and shininess around the edges of the holes. This is a clear sign of new bone growth and evidence that the person whose skull was opened not only survived the operation but lived months or even years afterwards while the bone regrew.
Having one's skull opened in a modern surgical setting is not taken lightly, even with the most modern surgical techniques. The prospect of undergoing the operation in the late Stone Age may appear to us to imply certain death. However, the survival rate of the operation was quite high. Close examination of archeological findings suggests that 75% of those who underwent the procedure lived long enough for new bone to grow around the opening. That number is actually higher than the survival rate for brain surgery during the nineteenth century, when Stone Age trepanned skulls were first identified. Brain surgery during the mid-1860s frequently resulted in infections that killed up to 75% of patients.
Trepanned skulls have been found all over the world, including sites in Peru, China, India, and France, and parts of the Middle East and Africa. While trepanning is an effective surgical technique for relieving pressure on the brain caused by bleeding, most archeologists suspect the operation was carried out in the Stone Age to achieve a different goal. Trepanning, they suspect, was performed to release evil spirits or demons, which the shamans or witch doctors of the time believed produced symptoms of what we know as mental disorders and, perhaps, diseases of the brain. The instruments used in trepanning were likely to have been made of obsidian, a very hard, glasslike, volcanic rock that can hold a very sharp cutting edge. There is also evidence that the end of a wooden stick, hardened by fire and turned back-and-forth rapidly while pressed against the skull may have served as a primitive, but effective, surgical drill.
Neuroscientist and author Elliot Valenstein believes that trepanning did not amount to intentional brain surgery. He quotes from the Latin text by the twelfth-century surgeon Roger of Salerno, who wrote: "For mania and melancholy, the skin of the top of the head should be incised in a cruciate fashion and the skull perforated to allow matter to escape."
A curious example of what might be called pseudopsychosurgery occurred during the Middle Ages. Some unscrupulous individuals wandered across Europe convincing gullible people that mental disorders were caused by a "stone of madness." To fool others, these quacks faked operating on the brains of mentally ill individuals and, using sleight-of-hand, appeared to produce a real stone from the victim's head, thus "proving" their claim and effecting a "cure." No doubt, these frauds quickly moved on to other towns before their patients showed signs of continuing psychiatric symptoms.
The impetus for developing a radical treatment
Unfortunately, effective treatments for mental illnesses remained unavailable until the second half of the twentieth century. Before then, psychiatric "care" consisted mostly of imprisonment, neglect , restraint, and/or punishment. During the eighteenth century, more humane conditions of confinement were introduced, but effective treatments remained unavailable. Physicians were desperate for treatments that might make it easier to control violent and deranged patients.
By the end of the nineteenth century, researchers became aware of the role played by the frontal cortex—a part of the brain located behind the forehead—in behavior control. They discovered from the results of animal experiments and observing humans who suffered damage to this part of the brain that the frontal lobes affect emotions and behavior. This bit of knowledge, combined with the development of effective anesthesia, led to the first modern instances of psychosurgery during the 1890s. A Swiss surgeon named Gottlieb Burkhardt deliberately damaged the frontal lobes of six psychiatric patients in hopes of relieving psychiatric symptoms; at least one of his subjects died and the experimental surgery was discontinued amid criticism from other physicians.
Psychosurgery in the twentieth century
PREFRONTAL LEUCOTOMY. In 1900, an Estonian surgeon, Lodivicus Pussepp, picked up where Burkhardt left off. He cut nerve tracks leading from the frontal lobes to other parts of the brain in psychiatric patients, with unimpressive results. A decade later, he injected tissue-destroying chemicals into the frontal lobes of mentally ill patients through holes drilled over the frontal lobes. Although the procedure accomplished little or nothing in the way of therapy, Pussepp remained optimistic about the ability of this procedure to improve the condition of psychiatric patients. Interest in the frontal lobes as a target for treating mental disorders continued on a small scale until the heyday of psychosurgery began in the 1930s.
In 1935, researchers in the United States reported that damaging the frontal lobes and a nearby region of the brain called the prefrontal cortex could pacify a previously aggressive chimpanzee. A Portuguese psychiatrist , Antonio Egas Moniz, learned of these results and recruited neurosurgeon Almeida Lima to operate on some humans suffering from severe psychoses. Moniz's aim was to disconnect nerve pathways running from the frontal lobes to a part of the brain called the thalamus, which is located closer to the center of the brain. By cutting these connections, Moniz hypothesized that he could disconnect a neural circuit that ran from the frontal cortex to the thalamus and then to other parts of the brain's surface. He hoped that interrupting this pathway would disrupt the repetitive thoughts that Moniz believed were responsible for psychotic symptoms.
But as Elliot Valenstein writes in his book Great and Desperate Cures, The Rise and Decline of Psychosurgery and Other Radical Treatments for Mental Illness , "Although Moniz' rationale for prefrontal leucotomy was so vague as to constitute no theory at all, his explanation was repeated so often that it—like the emperor's new clothes in Hans Christian Andersen's famous story— acquired a veneer of truth and was accepted (or at least repeated) by many other people." Psychiatrists were so desperate for a treatment for severe cases of mental illness that they allowed themselves to support the use of a procedure that was unproven and increasingly subject to abuse.
Moniz and Lima called their procedure leucotomy. It involved trepanning the skull, one hole on each side of the head, inserting a wire knife and cutting the targeted nerve fibers. Results were mixed enough for Moniz to recommend that the procedure be reserved only for the most seriously mentally ill patients for whom no other course of care or treatment worked. Nevertheless, after 1936, use of the technique spread rapidly, with equally unimpressive results overall. With little evidence of effectiveness and facing opposition from many psychiatrists, particularly psychotherapists, the technique would probably have been abandoned were it not for a pair of American physicians who revived the questionable procedure.
THE PREFRONTAL LOBOTOMY. American neurologist Walter Freeman and neurosurgeon James Watts began operating on patients in 1936 and soon began aggressively promoting its effectiveness. Eventually, they overcame doubts expressed by their colleagues who somewhat reluctantly accepted the procedure now referred to as prefrontal lobotomy. In 1946, Freeman simplified Moniz's leucotomy procedure, reducing it to a less complicated, less messy, and less time-consuming operation known as the "ice-pick lobotomy." This allowed Freeman to line up patients and, under local anesthesia, tap an ice pick through the thin bone on the roof of their eye sockets. With the ice pick in the brain, Freeman would sweep it back and forth to cut the frontal lobe's connections to the rest of the brain. This in-and-out procedure required no hospitalization but many physicians viewed it with alarm. Watts himself refused to cooperate with Freeman after this technique was developed.
Still, in the 1940s, U.S. physicians performed an estimated 18,000 lobotomies. It was equally popular in other countries where more than 50,000 operations were conducted during the same period. Sadly, Moniz's warning was forgotten. The procedure was not reserved for the most hopeless cases but instead applied to "difficult" patients and became a way to control behavior rather than to relieve symptoms of mental disorder. The abuse often bordered on the criminal. Yet, Moniz received the 1949 Nobel Prize for Medicine and Physiology for pioneering the procedure.
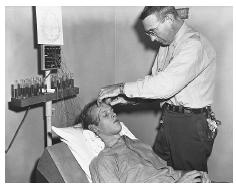
Fortunately, but still too late, critics of the operation began to convince others that there was no scientific proof that lobotomies helped mentally ill patients. It could certainly calm violent patients but it did so at a terrible cost. As one nurse who recently treated an aged patient who had been lobotomized years before said, "You look in her eyes and you see there is no one there." Victims of the procedure lack emotions, ambition, social skills, and the ability to plan. The operation was used to control the mentally ill and others, such as uncontrollable children and political dissidents, whose behavior did not conform to society's standards. Arguments against the procedure were powerful: it permanently and severely damaged the brain and often produced unreactive, lifeless individuals whose personalities were forever destroyed. With the introduction of psychotherapeutic drugs—especially chlorpromazine (Thorazine)—in the mid-1950s, lobotomies fell out of fashion.
Psychosurgery today
No one advocates the use of classical lobotomies today as a treatment for mental disorders. However, a small minority of neurologists advocates the use of very precise surgical techniques to produce small lesions in defined areas of the brain to treat rare cases of severe mental illness such as life-threatening depression or incapacitating anxiety or obsessions. However, there is little need for such procedures today. Antipsychotic and antidepressant medications are the treatments of choice for treating mental disorders. Mainstream medicine now classifies psychosurgery as an experimental procedure, and many rules exist to protect patients who might be subjected to it. The majority of mental health professionals believe that psychosurgery is either never justified or should only be considered as a last resort, to be reserved for the most extreme cases of untreatable mental disease when all other therapies have failed.
Resources
BOOKS
Pressman, Jack D. Last Resort: Psychosurgery and the Limits of Medicine. New York, NY: Cambridge University Press, 1998.
Valenstein, Elliot S. Great and Desperate Cures, The Rise and Decline of Psychosurgery and Other Radical Treatments for Mental Illness. New York: Basic Books, 1986.
Valenstein, Elliot S., ed. The Psychosurgery Debate. San Francisco: W.H. Freeman, 1980.
Woods, Michael and Mary B. Woods. Ancient Medicine, From Sorcery to Surgery. Minneapolis: MN: Runestone Press, 2000.
ORGANIZATIONS
American Psychiatric Association. 1400 K Street NW, Washington D.C. 20005. <http://www.psych.org> .
Dean A. Haycock, Ph.D.
Comment about this article, ask questions, or add new information about this topic: